Postpartum Depression: Recognizing Symptoms, Treatment, and Self-Care
Postpartum depression (PPD) is a mental health condition that affects many new mothers and can impact men as well. Unlike the “baby blues,” which are short-lived mood changes post-birth, PPD is more intense, longer-lasting, and requires a more structured treatment approach. This article covers everything you need to know about PPD, from symptoms and treatments to self-care strategies, with a focus on early diagnosis and effective interventions.
Can Men Have Postpartum Depression?
Yes, men can experience postpartum depression, even though it’s less commonly discussed. Around 10% of fathers face symptoms of PPD, which may look different from those of mothers. Common symptoms in men include irritability, fatigue, and withdrawal from family, which can stem from stress, sleep deprivation, and increased responsibilities.
It’s important to address male PPD because it can affect family dynamics and the mental well-being of both parents. Men experiencing PPD can benefit from support groups, counseling, and open communication with their partners.
Postpartum Depression Test
Early diagnosis of PPD is essential for effective treatment, and tests such as the Edinburgh Postnatal Depression Scale (EPDS) help identify symptoms. This test is a brief self-assessment used by healthcare providers to detect signs of depression or anxiety.
The EPDS consists of questions about mood, thoughts, and emotional well-being. Individuals scoring above a certain threshold are often advised to seek a professional mental health evaluation. Online versions of the EPDS are also available and can provide insight, though they are not a substitute for a clinical diagnosis. If you or a loved one notices signs of persistent sadness, irritability, or detachment from the baby, consider consulting a healthcare provider for further guidance.
How to Prevent Postpartum Depression
While it isn’t always possible to prevent PPD due to its biological and hormonal influences, you can reduce risk factors through proactive self-care and mental health support.
- Practice Self-Care: Prioritizing rest, balanced meals, and regular exercise can support your mental and physical well-being. Since sleep deprivation is common for new parents, alternating sleep schedules with your partner can be beneficial.
- Stay Connected: Strong social support is a key factor in mental health. Reaching out to family and friends for assistance with childcare or emotional support can help you manage stress and feel less isolated.
- Prepare Mentally: If you have a history of depression or anxiety, working with a therapist during pregnancy can help manage symptoms before they become severe. Early counseling and monitoring can reduce the likelihood of developing full-blown PPD.
- Manage Expectations: Adapting to a new routine with a baby can be overwhelming. Setting realistic goals and asking for help when needed can relieve stress.
- Avoid Social Isolation: New parents often feel isolated, which can worsen their mood. Consider joining a new parents’ support group or taking the baby for short outings to stay connected with the outside world.
By adopting these preventative measures, you can lower your risk of severe PPD symptoms and foster a more positive postpartum experience.

Postpartum Depression Pill
The postpartum depression pill, Zuranolone, is a recent breakthrough in PPD treatment. Unlike traditional antidepressants, which can take several weeks to work, Zuranolone is designed for rapid relief, often showing effects within a few days. This short-term medication is taken over two weeks and helps regulate the neurochemicals related to mood.
Zuranolone may be an option for those who find it challenging to access consistent mental health care or need quick relief. However, like any medication, it’s essential to consult a healthcare provider to discuss whether it’s suitable, especially if combined with therapy or other treatments for maximum effectiveness.
Postpartum Depression Self-Care
In addition to professional treatment, self-care plays a significant role in managing postpartum depression. These practices can make a big difference in daily mood and overall mental health.
- Establish a Routine: Creating a simple routine helps bring stability. Small tasks, such as showering or preparing a nutritious snack, can be empowering and establish a sense of accomplishment.
- Practice Mindfulness: Simple mindfulness exercises, like deep breathing or meditation, can help reduce stress and improve mental clarity. Mindfulness can also encourage you to stay present and calm, which is beneficial during challenging parenting moments.
- Set Healthy Boundaries: Setting boundaries with visitors or family can reduce the pressure and give you space to adjust. Politely declining or postponing social events that feel overwhelming is essential for self-care.
- Reduce Social Media: Social media can lead to unrealistic comparisons with others’ lives, which may contribute to feelings of inadequacy. Limiting social media time can help you maintain a more balanced self-view.
- Engage in Enjoyable Activities: Find short periods to do things you enjoy, like reading, painting, or listening to music. Engaging in activities you love provides a sense of joy and relaxation.
These self-care strategies support overall mental health, helping individuals better manage PPD symptoms alongside professional treatments.
How Does Therapy Help in the Treatment of Depression?
Therapy is a highly effective treatment for postpartum depression, providing individuals with coping tools and a space to process their feelings. Here are some therapy options commonly used in treating PPD:
- Cognitive Behavioral Therapy (CBT): CBT is a practical therapy that addresses negative thinking patterns. It empowers individuals to replace harmful thoughts with healthier ones and set achievable goals for daily life.
- Interpersonal Therapy (IPT): IPT focuses on relationship challenges, which can be heightened during the postpartum period. It helps individuals navigate the changes in family dynamics and adjust to their new role as a parents.
- Group Therapy: Group sessions connect individuals experiencing similar struggles, creating a supportive environment. Many people find comfort in sharing experiences and receiving encouragement from others facing similar challenges.
- Psychodynamic Therapy: This therapy delves into the deeper, unconscious factors influencing mental health. By exploring past experiences and emotional patterns, individuals gain insights that promote healing.
Therapy provides essential guidance and a safe environment to work through complex emotions, helping individuals recover from PPD more effectively.
Conclusion
Postpartum depression is a treatable mental health condition that affects many new parents. By understanding its symptoms, exploring treatment options, and adopting self-care practices, individuals can manage PPD and improve their quality of life. For those experiencing signs of PPD, reaching out to healthcare providers for support is a crucial first step toward recovery. With a combination of medical interventions, therapy, and self-care, new parents can navigate the challenges of PPD and build a healthier, happier future for themselves and their families.
What is postpartum depression, and how is it different from the “baby blues”?
Postpartum depression (PPD) is a form of depression that occurs after childbirth, characterized by persistent feelings of sadness, fatigue, anxiety, and emotional distress that can affect daily functioning and bonding with the baby. It’s more intense and long-lasting than the “baby blues,” a milder and temporary state of mood swings, crying spells, and irritability that usually resolves within two weeks after birth. PPD can last for months if left untreated and may require medical intervention.
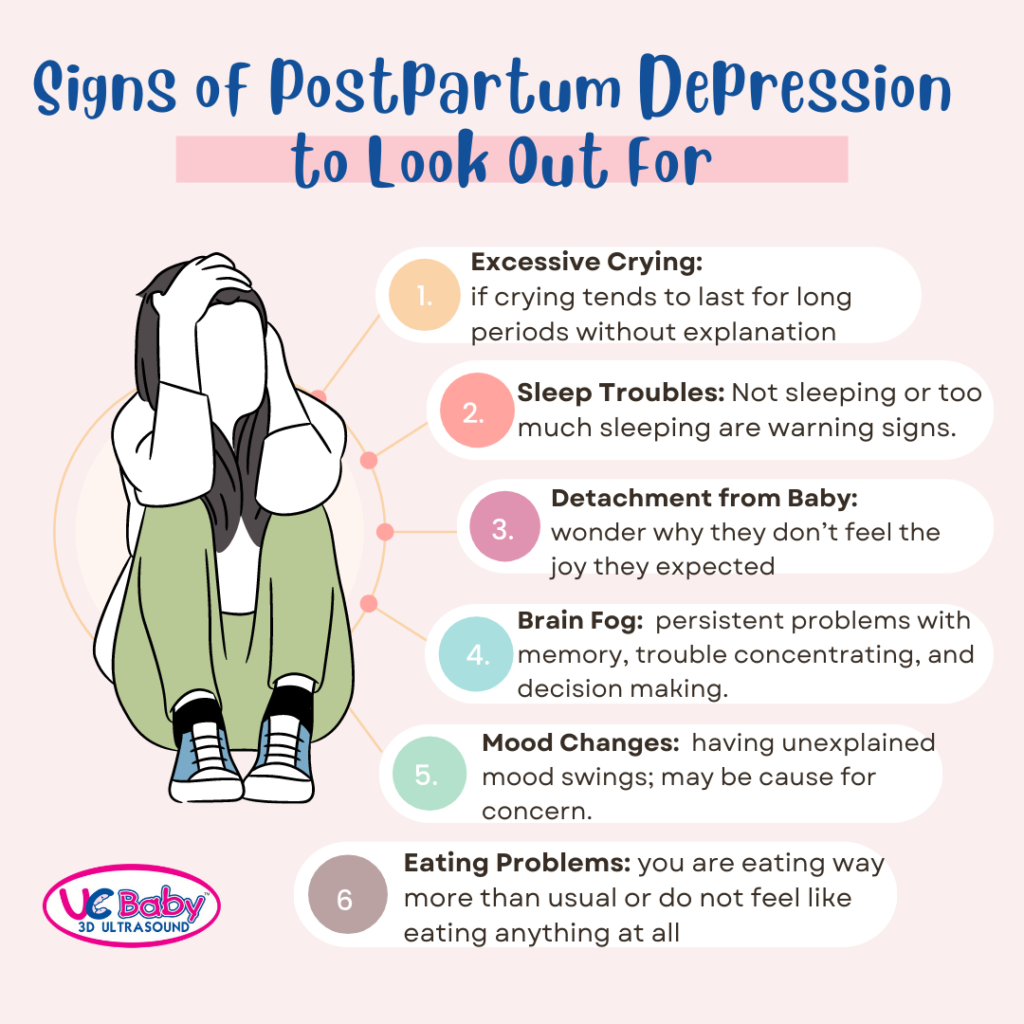
What are the symptoms of postpartum depression?
Symptoms of postpartum depression include severe mood swings, overwhelming fatigue, feelings of worthlessness or guilt, difficulty bonding with the baby, anxiety, withdrawal from loved ones, and in severe cases, thoughts of self-harm or harming the baby. Unlike the baby blues, these symptoms are intense and persistent, significantly affecting a new parent’s daily life and well-being.
Can postpartum depression affect fathers as well?
Yes, men can experience postpartum depression. Fathers may experience symptoms of irritability, sadness, fatigue, and withdrawal due to lifestyle changes, lack of sleep, and increased responsibility. Approximately 10% of new fathers are affected by PPD. While their symptoms may look different, their mental health is just as crucial to the well-being of the family and should be addressed.
How can postpartum depression be treated?
Postpartum depression is treated with a combination of methods, including counseling, medication, and support groups. Common therapies, like cognitive behavioral therapy (CBT) and interpersonal therapy (IPT), help address the symptoms and teach coping strategies. In cases of moderate to severe PPD, antidepressant medications or, in some cases, the new postpartum-specific medication Zuranolone, can offer additional support under the supervision of a healthcare provider.
Can postpartum depression be prevented?
While there’s no guaranteed way to prevent postpartum depression, certain practices can reduce the risk. These include establishing a strong support system, practicing self-care during and after pregnancy, seeking mental health support if there is a history of depression or anxiety, and setting realistic expectations for parenting. Early intervention and open communication with loved ones can help mitigate the effects of postpartum depression if symptoms begin to emerge.